2020年紐約頒布的一項新法律規定
大型團體醫療保險計劃必須涵蓋IVF(不孕不育症),並要求所有私人保險公司承擔醫療必需的卵子冷凍費用。
IVF醫療保險,IVF醫療保險由醫療保險承保,並且從2020年1月1日開始,如果您在一家擁有100名員工或以上的公司工作,就可以享受此項福利。
對於較小的團體(即少於100人的公司),您的保險可能會涵蓋I.U.I.
不孝有三,無後為大
但在現金社會,每個人都不得不為口奔馳,面對每天如此繁忙的工作,緊張的生活節奏,導致很多人都錯過了生育的黃金時機。正如本人,所以我清楚知道40歲前是生育最關鍵的時刻!
本人曾經在幾年前,大概是2015年的時候咨詢過長島的醫生關於人工受孕的事情,當時得到的信息是,他們有提供一種3萬多美元的套餐,就是說包生孩子,一直讓你嘗試到能成功懷上為止。當然這也已經是幾年前的價格,相信現在應該更貴一點。
而我也有個朋友在那些不孕不育的公司上班,她的醫生是常春藤名校畢業的,從他那裡得知的價格是4萬多美元了!
寫這篇文章的主要原因是,我們每個月都有接到好幾個客人是咨詢關於生育問題的,他們都想知道如何可以用保險來覆蓋人工受孕IVF (In vitro fertilization)
在過去多年來,我們也有提供資訊,有些保險公司會提供IUI (Intrauterine insemination),這是一種俗稱“生仔針”的藥物,可以大大提高懷孕的可能性,不過這支神奇的針價值不菲哦,需要幾千美元打一針。這對很多人來說,也不是容易接受的。
但新喜訊是,從2020年1月1日起,大型團體/公司(100人以上),政府要求其醫療保險需覆蓋3次嘗試人工受孕的費用。
如果按照一次2.5萬來算(相當於一輛小車的價格),那些能用得上這三次機會的女士,就等於免費有了三輛小車了。
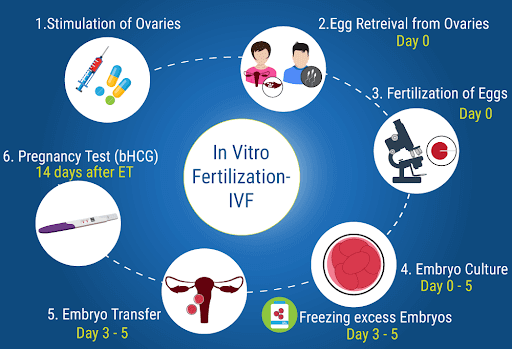
IVF 和IUI的主要分別是?
IUI和IVF治療之間的主要區別是:IVF是一個涉及卵子刺激,取回,受精和轉移的過程。 IUI將精子注入子宮,以減少精子到達卵子的時間。 將產生的胚胎轉移到子宮中。
紐約市覆蓋IVF嗎?
2020年國家預算中頒布的新法律規定,某些大型團體(100人以上)保險計劃必須涵蓋IVF,並要求所有私人保險公司承擔醫療必需的卵子冷凍。
《可負擔醫療法案》由於州法律的怪異,要求紐約承擔中小型計劃的任務。
紐約IVF的費用是多少?
紐約是治療IVF患者最昂貴的州之一,因為單個IVF週期的平均費用為24,000美元。根據我們的數據,只有不到38%的紐約州居民擁有涵蓋IVF相關費用的保險單,因此大多數患者完全自掏腰包。
如此昂貴的IVF值得嗎?
曾幾何時,很多人會考慮能否負擔得起IVF這般昂貴的費用。但現在在新政策的規定下,大家只需盡量爭取能去大公司上班(大公司的定義是員工多於100人),就能省下一大筆費用了。
而少於100人的小型公司,政府規定的是其醫療保險需要覆蓋冷凍卵子的費用。
能否通過IVF選擇嬰兒的性別?
原則上來說是可以的,人工受孕是可以決定孩子的性別,但請記得我們只是醫療保險代理人,並非醫生,所以請和相關專業人士確認。
但以我們自己的理解,關於選擇性別的費用是不包含在醫療保險計劃中的,意味著需要額外的費用。
下方我們也有提供現在最新的醫療保險公司所覆蓋的準則。
* 如果有人願意幫忙翻譯下文內容,我們可以把你的署名放在此文章中,以幫助到有需要人士。
紐約不孕不育者喜訊 – New York IVF Mandate
In this Aug. 11, 2008, file photo, a scientist works during an IVF process. A new law, enacted in the 2020 New York state budget, mandates that certain large-group insurance plans cover IVF, and requires all private insurance companies to cover medically necessary egg freezing. (AP Photo/PA, Ben Birchall, File)
ALBANY — With more young women and men delaying parenthood, the demand for fertility treatments such as egg freezing and in-vitro fertilization (IVF) has grown across the country.
Legislation and science have lagged behind the trend, and the cost of the treatments can be prohibitively expensive.
A new law, enacted in the 2020 state budget, mandates that certain large-group insurance plans cover IVF, and requires all private insurance companies to cover medically necessary egg freezing.
It is projected to benefit to up to 2.4 million New Yorkers, according to figures from Gov. Andrew M. Cuomo’s administration, but there are kinks to iron out before it guarantees coverage to the other half of insured New Yorkers, including gay men, Medicaid-recipients, and the self-employed.
Secretary to the Governor Melissa DeRosa, the first woman to hold that position, pushed for IVF legislation in the spending plan, citing it as a top priority for the two-year-old Council for Women and Girls.
DeRosa, 36, said that she understands the anxiety of women in her age group who are pressured to decide between advancing their careers and starting a family.
“There is nothing more personal or life altering than the ability to conceive and making the choice about when to conceive,” DeRosa said. “As someone who is currently facing these life-altering decisions, I know firsthand the toll they take — emotionally and financially.”
Last year, Cuomo directed the state Department of Financial Services to study the cost of implementing an insurance mandate on egg freezing and IVF.
The report, released to the public in February, suggests that mandating all insurances cover those costs would be too expensive for the state. The Affordable Care Act, due to a quirk in state law, requires New York to absorb mandates on small and medium sized plans.
“Limiting an IVF mandated benefit to large group insurance policies mitigates that premium impact and avoids a state fiscal risk,” according to the DFS report.
Ten states have IVF insurance coverage laws, according to the DFS study, but most include limits on funding, number of cycles, age, and other restrictions.
In addition, providing access to treatment for thousands of New Yorkers, the bill is “finally a recognition that infertility is a disease, not a lifestyle choice,” said Barbara Collura, President & CEO of RESOLVE: The National Infertility Association. “Quite honestly, having New York do it is going to be a game-changer for the rest of the country.”
Highlights of the new law:
What type of plans must offer coverage?
Large insurance plans, providing coverage to 100 employees or more, must cover in-vitro treatments and associated medications and testing.
Employees of small and medium-sized companies, companies that self-insure, and those with individual insurance plans are not guaranteed coverage. Approximately half of New Yorkers with health insurance would qualify for the benefit, according to DFS.
How many cycles of IVF are covered?
Three.
Are their age restrictions?
No. New York’s law gives the doctor discretion to consider the patient’s age when deciding if she is an appropriate candidate for IVF.
What about egg freezing?
The new mandate requires all insurance plans cover cryogenic egg freezing for medically necessary purposes. Women undergoing chemotherapy for cancer are often offered the opportunity to freeze their eggs, but decline when they learn of the cost, according to the DFS report.
Other qualifying procedures include sex-reassignment surgery, sickle cell anemia, bone marrow transplant, or surgery for endometriosis.
Is surrogacy covered under this plan?
No. Currently, surrogacy is illegal in New York.
Insurers are also not mandated to cover the healthcare of a person outside the family unit.
Sen. Brad Hoylman, D-Manhattan, and Assemblywoman Amy Paulin, D-Westchester, have introduced legislation updating the state’s surrogacy laws. If it passes, the issue will be revisited.
“We want to probably seek some guidance from the Department of Health … and work with experts in making certain that the bill is carefully crafted,” Hoylman said.
Are single women and gay and lesbian couples covered under the plan?
Single women and lesbians are covered. For gay men, it’s complicated.
IVF mandates in other states have excluded gay and lesbian couples due to narrow medical definitions of infertility. Anti-discrimination language in the bill prohibits discrimination based on marital status, age, sexual orientation or gender identity, and broadens that definition.
Infertility, according to the bill, is a condition characterized by an inability to conceive “after 12 months of regular, unprotected sexual intercourse or donor insemination.” For women above the age of 35, the requirement is six months of regular, unprotected sexual intercourse or donor insemination without conception.
Figuring out how to extend the benefit to male couples, who can only conceive through an out-of-state surrogate, has not been worked out, according to Hoylman.
“The issue is, for example, a gay couple who is seeking a donor egg, whether fertilizing the egg in the transfer would be covered,” Hoylman said. “I’ll be looking at the language to strengthen it.”
What other programs are out there to assist with fertility treatments?
In 2003, the state’s Infertility Demonstration Program was created to subsidize the cost of fertility treatments for employed New Yorkers. Grants are available on a sliding scale, based on income for families earning up to $195,000.
To qualify, patients must be between the ages of 21 and 44 years and have private health insurance (not Medicaid, Medicare, or Family Health Plus).
聯合牛津不孕不育 – Oxford Infertility Treatment
We Cover services for the diagnosis and treatment (surgical and medical) of infertility. “Infertility” is a
disease or condition characterized by the incapacity to impregnate another person or to conceive, defined
by the failure to establish a clinical pregnancy after 12 months of regular, unprotected sexual intercourse
or therapeutic donor insemination, or after six (6) months of regular, unprotected sexual intercourse or therapeutic donor insemination for a female 35 years of age or older. Earlier evaluation and treatment
may be warranted based on a Member’s medical history or physical findings. Such Coverage is available
as follows:
1. Basic Infertility Services. Basic infertility services will be provided to a Subscriber who is an
appropriate candidate for infertility treatment. In order to determine eligibility, We will use guidelines
established by the American College of Obstetricians and Gynecologists, the American Society for
Reproductive Medicine, and the State of New York.
Basic infertility services include:
• Initial evaluation;
• Semen analysis;
• Laboratory evaluation;
• Evaluation of ovulatory function;
• Postcoital test;
• Endometrial biopsy;
• Pelvic ultrasound;
• Hysterosalpingogram;
• Sono-histogram;
• Testis biopsy;
• Blood tests; and
• Medically appropriate treatment of ovulatory dysfunction.
Additional tests may be Covered if the tests are determined to be Medically Necessary.
2. Comprehensive Infertility Services. If the basic infertility services do not result in increased fertility,
We Cover comprehensive infertility services.
Comprehensive infertility services include:
• Ovulation induction and monitoring;
• Pelvic ultrasound;
• Artificial insemination;
• Hysteroscopy;
• Laparoscopy; and
• Laparotomy.
3. Fertility Preservation Services. We Cover standard fertility preservation services when a medical treatment will directly or indirectly lead to iatrogenic infertility. Standard fertility preservation services include the collecting, preserving, and storing of ova, sperm or embryos. “Iatrogenic infertility” means
an impairment of Your fertility by surgery, radiation, chemotherapy or other medical treatment affecting reproductive organs or processes.
4. Exclusions and Limitations. We do not Cover:
• In vitro fertilization; • Gamete intra-fallopian tube transfers or zygote intra-fallopian tube transfers;
• Costs for an ovum donor or donor sperm;
• Sperm and ova storage costs except when performed as fertility preservation services;
• Cryopreservation and storage of embryos;
• Ovulation predictor kits;
• Reversal of tubal ligations;
• Reversal of vasectomies;
• Costs for and relating to surrogate motherhood;
• Cloning; or
• Medical and surgical procedures that are experimental or investigational, unless Our denial is
overturned by an External Appeal Agent.
All services must be provided by Providers who are qualified to provide such services in accordance
with the guidelines established and adopted by the American Society for Reproductive Medicine. We will
not discriminate based on Your expected length of life, present or predicted disability, degree of medical
dependency, perceived quality of life, other health conditions, or based on personal characteristics
including age, sex, sexual orientation, marital status or gender identity, when determining coverage under this benefit.
第一保健不孕不育 – Healthfirst Infertility Treatment
We Cover services for the diagnosis and treatment (surgical and medical) of infertility when such infertility is the result of malformation, disease or dysfunction. Such Coverage is available as follows:
1. Basic Infertility Services. Basic infertility services will be provided to a Member who is an appropriate candidate for infertility treatment. In order to determine eligibility, We will use guidelines established by the American College of Obstetricians and Gynecologists, the American Society for Reproductive Medicine, and the State of New York. However, Members must be between the ages of 21 and 44 (inclusive) in order to be considered a candidate for these services.
Basic infertility services include:
• Initial evaluation;
• Semen analysis;
• Laboratory evaluation;
• Evaluation of ovulatory function;
• Postcoital test;
• Endometrial biopsy;
• Pelvic ultra sound;
• Hysterosalpingogram;
• Sono-hystogram;
• Testis biopsy;
• Blood tests; and
• Medically appropriate treatment of ovulatory dysfunction.
Additional tests may be Covered if the tests are determined to be Medically Necessary.
2. Comprehensive Infertility Services. If the basic infertility services do not result in increased fertility, We Cover comprehensive infertility services.
Comprehensive infertility services include:
• Ovulation induction and monitoring;
• Pelvic ultra sound;
• Artificial insemination;
• Hysteroscopy;
• Laparoscopy; and
• Laparotomy.
3. Exclusions and Limitations. We do not Cover:
• In vitro fertilization, gamete intrafallopian tube transfers or zygote intrafallopian tube transfers;
• Costs for an ovum donor or donor sperm;
• Sperm storage costs;
• Cryopreservation and storage of embryos;
• Ovulation predictor kits;
• Reversal of tubal ligations;
• Reversal of vasectomies;
• Costs for and relating to surrogate motherhood (maternity services are Covered for Members acting as surrogate mothers);
• Cloning; or
• Medical and surgical procedures that are experimental or investigational, unless Our denial is overturned by an External Appeal Agent.
All services must be provided by Providers who are qualified to provide such services in accordance with the guidelines established and adopted by the American Society for Reproductive Medicine.
L. Infusion Therapy.
We Cover infusion therapy which is the administration of drugs using specialized delivery systems that otherwise would have required You to be hospitalized. Drugs or nutrients administered directly into the veins are considered infusion therapy. Drugs taken by mouth or self-injected are not considered infusion therapy. The services must be ordered by a physician or other authorized Health Care Professional and provided in an office or by an agency licensed or certified to provide infusion therapy. Any visits for home infusion therapy count toward Your home health care visit limit.
Arkansas IVF Mandate
The Arkansas infertility mandate, enacted in 1987, requires at least $ 15,000-lifetime coverage for IVF (In Vitro Fertilization) treatment for infertility provided a woman’s eggs are fertilized by her husband’s sperm.
California IVF Mandate
California law requires insurers to offer infertility benefits to employers as an additional rider when they purchase their yearly insurance benefits. If your current employer does not offer infertility as part of your benefits package, this could be an area you could influence future benefits decisions
Connecticut IVF Mandate
The State of Connecticut passed a bill in 2005 which passed breakthrough legislation that requires most insurance companies to cover infertility diagnosis and treatment. … As of January 01, 2016 insurance carriers are required to remove the age limit on infertility benefits and policies.
Hawaii IVF Mandate
The Hawaii infertility mandate, enacted in 1989, requires any fertility coverage, including a single IVF cycle, in any plan that also provides maternity coverage for couples who have been trying unsuccessfully to conceive for 5 years or who have been diagnosed with a condition known to cause infertility.
Illinois IVF Mandate
The state of Illinois passed the Family Building Act in 1991. In short, it requires group health insurance plans that cover more than 25 employees to cover the diagnosis and treatment of infertility up to and including 4 IVF attempts (egg retrieval procedures).
Louisiana IVF Mandate
Know your rights: The Louisiana Infertility Mandate. The Louisiana infertility mandate, enacted in 2002, makes it illegal to exclude coverage for a medical condition just because it results in infertility. It does not require coverage for fertility drugs, treatments or sterilization (getting vasectomy or tubes tied).
Maryland IVF Mandate
This handout describes the Mandatory Benefits that may be contained in your contract if you have coverage through a large group (groups of more than 50 employees) health benefit plan or are in a grandfathered plan. (Your plan is a grandfathered plan if you were in a plan on or prior to March 23, 2010, and the plan has not substantially changed.)
Massachusetts IVF Mandate
The Massachusetts infertility mandate, enacted in 1987, is hailed as one of the most comprehensive in the country by requiring infertility be treated like any other medical condition and not mandating a cap on coverage (either in the number of cycles or a lifetime dollar amount).
Montana IVF Mandate
The Montana infertility mandate, enacted in 1987, requires HMOs to provide coverage for “infertility services” as a basic health care service that must be covered but it doesn’t define infertility or which services must be covered.
New Jersey IVF Mandate
New Jersey mandate for infertility coverage. … The insurance mandate states that any insurance provider who provides pregnancy-related benefits must also cover infertility treatment and IVF costs. The law also requires health plans contracting to cover state employees and teachers to include the same infertility coverage
Ohio IVF Mandate
The Ohio infertility mandate requires health maintenance organizations (HMOs) to provide basic health services, which includes infertility care, when medically necessary. A bulletin released by the department of insurance clarifies that IVF and other forms of assisted reproduction are outside of the scope of the law.
Rhode Island IVF Mandate
The Rhode Island insurance mandate states that insurance must provide coverage for medically necessary expenses for the diagnosis and treatment of infertility, which can include in vitro fertilization (IVF). But, the amount of coverage can vary from plan to plan.
Texas IVF Mandate
Texas state law requires certain insurers that cover pregnancy services to offer coverage for in vitro fertilization (IVF insurance benefits). … However, the law does not require those insurers to provide the coverage; nor does it force employers to include it in their health plans.
West Virginia IVF Mandate
West Virginia’s law requires health maintenance organizations to cover basic health care services, including infertility services, when medically necessary.